The aim is to ensure that all children with medical conditions, in terms of both physical and mental health, are properly supported in school so that they can play a full and active role in school life, remain healthy and achieve their academic potential.
The Academy will ensure that arrangements are in place to support pupils with medical conditions to enable them to access and enjoy the same opportunities at school as any other child. The focus will be on the needs of each individual child and how their medical condition impacts on their academy life. The policy aims to provide clear guidance and procedures to staff and parents.
The overall responsibility for ensuring the policy is implemented effectively is held by the Principal with support from the Deputy Principal
The Academy will work together with parents, pupils, local authorities, health professionals such as specialist nurses and other support services to ensure that children with medical needs receive a full education. In some cases, this will require flexibility and involve, for example, programmes of study that rely on part-time attendance at academy in combination with alternative provision. Consideration will be given to how children will be reintegrated back into the academy after periods of absence.
No child with a medical condition will be denied admission or prevented from taking up a place because arrangements for their medical condition have not been made. However, in line with our safeguarding duties, we will ensure that pupils’ health is not put at unnecessary risk from, for example, infectious diseases. We retain the right not to accept a child at academy at times where it would be detrimental to the health of that child or to others.
Students who are pregnant and require support with medications have an individual mother’s risk assessment, this will be updated to reflect any requests for support after consultation with parents.
The academy will work with parents where it has been brought to their attention that parents do not wish their child to be given medications, and individual assessments drawn up.
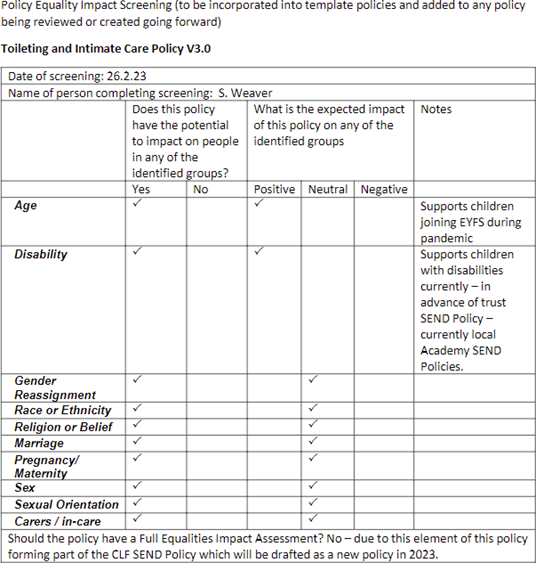
An equalities impact assessment has been carried out. The assessment concluded that there was potential adverse impact identified for some groups of people with protected characteristics and mitigations are in place to reduce that impact. The following equalities impact assessment report can be obtained from Jo Crickson.
This policy should be read alongside
Section 100 of the Children and Families Act 2014 places a duty on governing bodies of maintained schools, proprietors of academies and management committees of pupil referral units to make arrangements for supporting pupils at their academy with medical conditions.
Generally the Health and Safety at Work etc. Act 1974, and associated legislation, requires that organisations ensure the health and safety of persons at work and persons affected by their work. Pupils attending schools fall under this general legal requirement as they are affected by the work of the school whilst staff act in loco parentis, so are expected to do what a reasonable parent would do in given situations.
Additionally, the Equality Act 2010 legally protects people from discrimination in the workplace and in wider society. There is specific non-statutory advice ‘the Equality Act 2010 and Schools’ produced by the Department for Education to help schools to understand how the Equality Act affects them and how to fulfil their duties under the Act.
Guidance on the special educational needs and disability (SEND) system for children and young people aged 0 to 25, as detailed in the SEND Code of Practice
Statutory framework for the Early years foundation as amended Jan 2024
The roles and responsibilities set out below is not an exhaustive list and academies may want to add a wider range of people to their policy.
Local Authorities are commissioners of school nurses for maintained schools and academies. Under Section 10 of the Children Act 2004, they have a duty to promote co- operation between relevant partners such as governing bodies of maintained schools, proprietors of academies, clinical commissioning groups and NHS England, with a view to improving the wellbeing of children with regard to their physical and mental health, and their education, training, and recreation.
As such they should:
All records to support the request for supporting students with medical needs is confidential and should be stored securely in a lockable cabinet/ cupboard.
Only limited and applicable staff should have access to the cupboard with strict key control in place.
Any records held digitally should be secure with restricted access.
Must have parental/carer consent.
A record of medications dosage given on CPOMS.
Check of maximum dose and when previous dose was last taken.
The container is clearly labelled with the pupil’s name. The exception to this is the Academy may hold a bottle of Calpol or paracetamol tablets to be able to support a student with mild pain or discomfort with parental consent, and in line with other recording arrangements in place as normal practice. The parent must be informed of the age range of the Calpol Infant/ 6+) and sign to state they are happy on exception for this to be administered, a phone call be made first at time of administration to double check and for awareness.
Calpol and paracetamol, are for short term use only.
Administered for an agreed length of time, after which the medication will be returned to the parents.
Many pupils will need to take medication (or be given it) during the academy day at some time. Mostly, this will be for a short period only, to finish a course of antibiotics or apply a lotion. To support pupils with this will undoubtedly minimise the time they need to be off academy. Medication should only be taken in academy when absolutely necessary.
It is helpful if, where possible, medication can be prescribed in dose frequencies which enable it to be taken outside academy hours. Parents should be encouraged to ask the prescribing doctor or dentist about this.
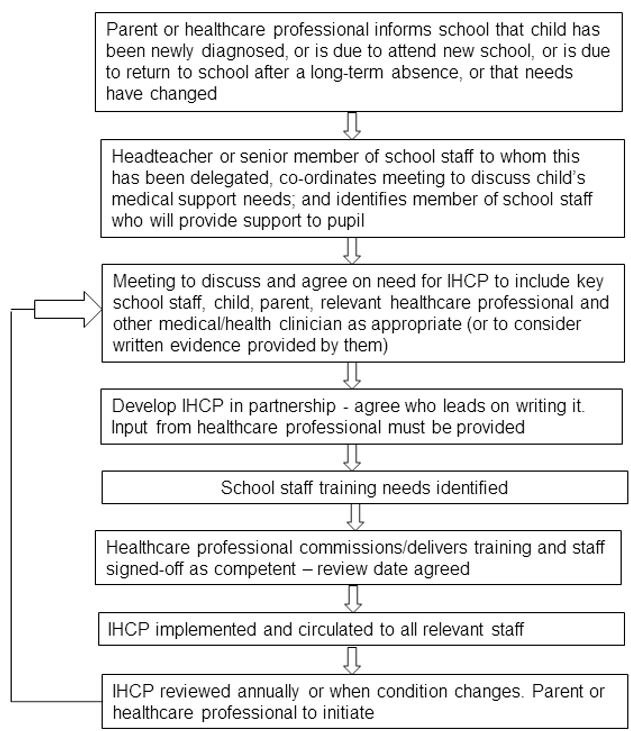
The following procedures are to be followed when notification is received that a pupil has a medical condition.
Lime Hills Academy students have an Education, Health and Care (EHC) plan which brings together health and social care needs, as well as their special educational provision. Where this is the case the IHCP should be linked to or become part of that statement or EHC plan.
The Academy will identify members of staff to support with the standard administration of medications, and awareness of procedures and paperwork/record keeping. The academy will arrange for these staff to attend managing medications training. Where there is a specific staff training need to support pupils with complex medical needs this will be identified by the specialist nursing team with a sufficient number of staff trained to ensure cover for sickness periods or staff turnover. A first aid certificate does not constitute appropriate training to support pupils with medical conditions.
Healthcare professionals commission, or delivers appropriate training and staff are signed off as competent. A review date for training will be agreed.
The IHCP will be implemented and circulated to all relevant staff. Supply staff will be informed that an IHCP is in place.
The IHCP will be monitored and reviewed annually or when the medical condition changes. The parent or healthcare professional may initiate the review.
For children starting at a new academy, arrangements should be in place in time for the start of the relevant academy term. In other cases, such as a new diagnosis or children moving to a new school mid-term, every effort will be made to ensure that arrangements are put in place within two weeks.
Not all pupils with medical needs will require an IHCP. The academy, together with the healthcare professional and parent will agree, based on evidence, whether a health care plan would be inappropriate or disproportionate. If consensus cannot be reached, the Principal will take the final view.
The following will be considered when deciding what information will be recorded on IHCPs:
Any member of staff providing support to a pupil with medical needs should have received suitable training. Where staff already have some knowledge of specific support needed by a child extensive training may not be required. Staff who provide support to pupils with medical conditions should be included in meetings where this is discussed.
The relevant healthcare professional should normally lead on identifying the type and level of training required, and how this can be achieved.
Training should be sufficient to ensure that staff are competent and have confidence in their ability to support pupils with medical conditions and to fulfil the requirements as set out in IHCPs. They will need an understanding of the specific medical conditions they are being asked to deal with, their implications and preventative measures.
Staff MUST NOT give prescription medicines under healthcare procedures without appropriate training (updated to reflect any IHCPs). In some cases, written instructions from the parent or on the medication container dispensed by the pharmacist may be considered sufficient, CLF require all staff who administer medications to undertake managing medications training, and to have specific training to support with specific medical needs, e.g. Diabetes, asthma, anaphylaxis and other more complex needs, having taken into consideration the training requirements as specified in pupils’ IHCPs.
Health care professionals, including the school nurse, can provide confirmation of the proficiency of staff in a medical procedure, or in providing medication.
All staff to receive awareness training of the academy’s policy for supporting pupils with medical conditions and their role in implementing that policy. This will also form part of staff induction training.
Following discussions with parents and where a child is deemed competent to manage their own health needs and medicines, this should be encouraged and this should be reflected within IHCPs.
Wherever possible, children should be allowed to carry their own medicines and relevant devices or should be able to access their medicines for self-medication quickly and easily, but with an appropriate level of supervision.
If a child refuses to take medicine or carry out necessary procedure, staff should not force them to do so, but follow the procedure agreed in the IHCP. Parents should be informed so that alternative options can be considered and a record should be kept.
Medicines will only be administered at school when it would be detrimental to a child’s health or school attendance not to do so.
No child under 16 will be given prescription or non-prescription medicines without their parent’s written consent.
Non-prescribed medicines may be administered under the following circumstances:
No child under the age of 16 will be given medicine containing aspirin unless prescribed by a doctor.
Where clinically possible medicines should be prescribed in dose frequencies which enable them to be taken outside academy hours.
The academy will only accept prescribed medicines that are in-date, labelled with the child’s name, provided in the original container as dispensed by a pharmacist. This will include instruction for administration, dosage and storage. Exceptions to this are over-the-counter medication where agreed protocols are agreed as above in point 2 and insulin which may be in a pen or pump but it must still be in date.
All medicines held by the academy to be stored will be kept in a lockable cupboard/fridge inside a lockable room which in a location which is known and accessible to the child. Where relevant the child should know who holds the key to the storage facility. Medicines such as asthma inhalers must always be readily available to the child and not locked away. This is particularly important when outside the premises e.g. academy trips.
Whilst DFE allows in some circumstances pupils to carry controlled drugs prescribed to them, in this Academy controlled drugs that have been prescribed will be securely stored with only named staff having access. A record will be kept of any doses used and the amount of the controlled drug held in academy.
Trained academy staff may administer a controlled drug to a child for whom it has been prescribed. Staff administering medicines should do so in accordance with the prescriber’s instructions.
The academy will keep a record of all medicines administered to individual children stating what, how and how much was administered, when and by whom. Any side effects should also be recorded.
When no longer required, medicines should be returned to parents to arrange for safe disposal. Medicines should also be returned to parents during holiday periods.
Each IHCP will clearly define what constitutes an emergency and explain what to do, including ensuring that all relevant staff are aware of emergency symptoms and procedures and where appropriate that other pupils know what to do if they think help is needed.
If a child is taken to hospital, a member of academy staff will stay with the child until the parent arrives.
From 1st October 2014 academies have been allowed to obtain, without a prescription, salbutamol inhalers, if they wish, for use in emergencies. Academies are not required to hold an inhaler – this is a discretionary power enabling schools to do this if they wish.
At Lime Hills, we do hold an emergency inhaler. Parents of asthmatic children will be asked to complete a form when their child joins the Academy giving permission for their child to use the Academy inhaler if required in an emergency situation, such as leaving their own at home or in the event of their own inhaler not working for some reason.
From 1 October 2017 the Human Medicines (Amendment) Regulations 2017 will allow all Academies to buy adrenaline auto-injector (AAI) devices without a prescription, for emergency use in children who are at risk of anaphylaxis but their own device is not available or not working (e.g. because it is broken, or out-of-date).
The academy’s spare AAI should only be used on pupils known to be at risk of anaphylaxis, for whom both medical authorisation and written parental consent for use of the spare AAI has been provided.
The academy’s spare AAI can be administered to a pupil whose own prescribed AAI cannot be administered correctly without delay.
A defibrillator is a machine used to give an electric shock to restart a patient’s heart when they are in cardiac arrest. The LHA Nailsea site has a defibrillator located in the main admin office. LHA WSM does not have its own defibrillator but there is a defibrillator accessible in the main reception area of WHA
This is the responsibility of the local authority. The academy will work with the local authority who may find it helpful to be aware of a pupil’s IHCP and what it contains, especially in respect of emergency situations.
The academy will actively support pupils with medical conditions to enable them to participate in academy trips and visits or in sporting activities, and not prevent them from doing so.
The academy will consider what reasonable adjustments they might make to enable children with medical needs to participate fully and safety on academy trips and visits. It is best practice to include this as part of the activity risk assessment to ensure that pupils with medical conditions are included.
All staff attending the trip will be aware of what constitutes an emergency and the procedures as follows.
If an emergency occurs on a school visit the following points need to be considered.
The following is regarded by the academy as unacceptable practice:
The CLF fully indemnifies staff who administer medication providing they are acting within the scope of their employment, have been provided with adequate training and are following the CLF policy/guidance for the purpose of indemnity.
Zurich Municipal Insurance Policy Number KSC-242115-5493
Customer Name Cabot Learning Federation
If parents or pupils are dissatisfied with the support provided by the academy to pupils with medical conditions, they should discuss their concerns directly with the academy. If the issue remains unresolved, they may make a formal complaint via the academy’s complaint procedure.
Please access the academy complaints policy HERE
Complaints can be sent to:
Academy Name: Lime Hills Academy Complaints Coordinator: Lynn Ovens
Contact details for Academy Complaints Coordinator: Lime Hills Academy, Pound Lane, Nailsea, BS48 2NN
The links to the DFE Template for:
· Health Care Plan
· Parental consent
· Record of medication given
· Training records
· Model letter inviting parents/carers to contribute to a health care plan
https://www.resus.org.uk/library/additional-guidance/guidance-anaphylaxis
https://www.anaphylaxis.org.uk/what-is-anaphylaxis/
All children at Lime Hills Academy have the right to be safe and be treated with dignity, respect and privacy at all times so as to enable them to access all aspects of learning and school life.
It is likely that children will be toilet trained before attending Lime Hills Academy. However, we are inclusive in our approach and will support children and families to make sure all children are able to participate in the Foundation Stage who may, for any reason, not yet be toilet trained and who may be wearing nappies or equivalent.
This policy sets out clear principles and guidelines on supporting intimate care with specific reference to toileting. It should be considered in line with our Safeguarding Policy, Health and Safety Policies, and must be read in conjunction with dealing with bodily fluids guidance in Health and Safety manual under infection control.
This policy supports the safeguarding and welfare requirements of the Early Years Foundation Stage (EYFS) 2017 and the Equalities Act 2010: Lime Hills Academy will ensure that:
This covers any tasks that involves the dressing and undressing, washing including intimate parts, helping someone use the toilet, changing nappies or carrying out a procedure that requires direct or indirect contact to an intimate personal area.
The staff team at Lime Hills Academy works in partnership with parents/carers to provide care appropriate to the needs of the individual. Toilet training is seen as a self-care skill that children have the opportunity to learn with the full support of all adults involved. Parents will be supported by the school to work in partnership towards their child’s toilet training unless there are medical or other developmental reasons why this may not be appropriate at the time. If children require regular changing, then a care plan will be created. The care plan will set out:
When intimate care is given, the member of staff tells a member of their team that they are providing intimate care and where they will be doing this. The door to the changing area will be left open whilst protecting the privacy of the child.
The member of staff explains fully, to the child, each task that is carried out, and the reason for it. Staff encourage children to do as much for themselves as they can, lots of praise and encouragement will be given to the child when they are successful in any aspect of self-care. Staff will not apply creams but will support the child to do it themselves if medically necessary.
All staff working in early years setting have a full DBS check, in line with all staff across the CLF.
Particular staff members will typically be identified to change a child with known toileting and intimate care needs. Staff will record the date and time when a child has been given intimate care and this will be shared with parents/carers.
Staff are trained on the signs and symptoms of child abuse through annual Safeguarding training within the Cabot Learning Federation. If a member of staff is concerned about any physical or emotional changes, such as marks, bruises, soreness, distress etc. they will inform the Designated Safeguarding Lead Officer (DSLO) immediately.
If a child makes an allegation against a member of staff, the principal must be informed immediately, and the procedure set out in the Safeguarding Policy will be followed.
Appropriate PPE will be used at all times, in line with guidance from Health and Safety teams. Urine, faeces, blood, and vomit will be cleaned up immediately and disposed of safely in the appropriate bins. Nappy bins will be available when a child is still wearing nappies. When dealing with body fluids, staff wear protective clothing, disposable plastic aprons and gloves and wash themselves thoroughly afterward. Soiled children’s clothing will be bagged to go home– staff will not rinse it. Children will be kept away from the affected area until the incident has been completely dealt with.
All staff maintain high standards of personal hygiene and will take all practicable steps to prevent and control the spread of infection.
This policy aims to manage risks associated with toileting and intimate care needs and ensures that employees do not work outside the remit of their responsibilities set out in this policy.
Signed by: Principal
Signed by: chair of Academy Council
Date: November 2024
Review Date: November 2026